Written by: Erik Prinsen
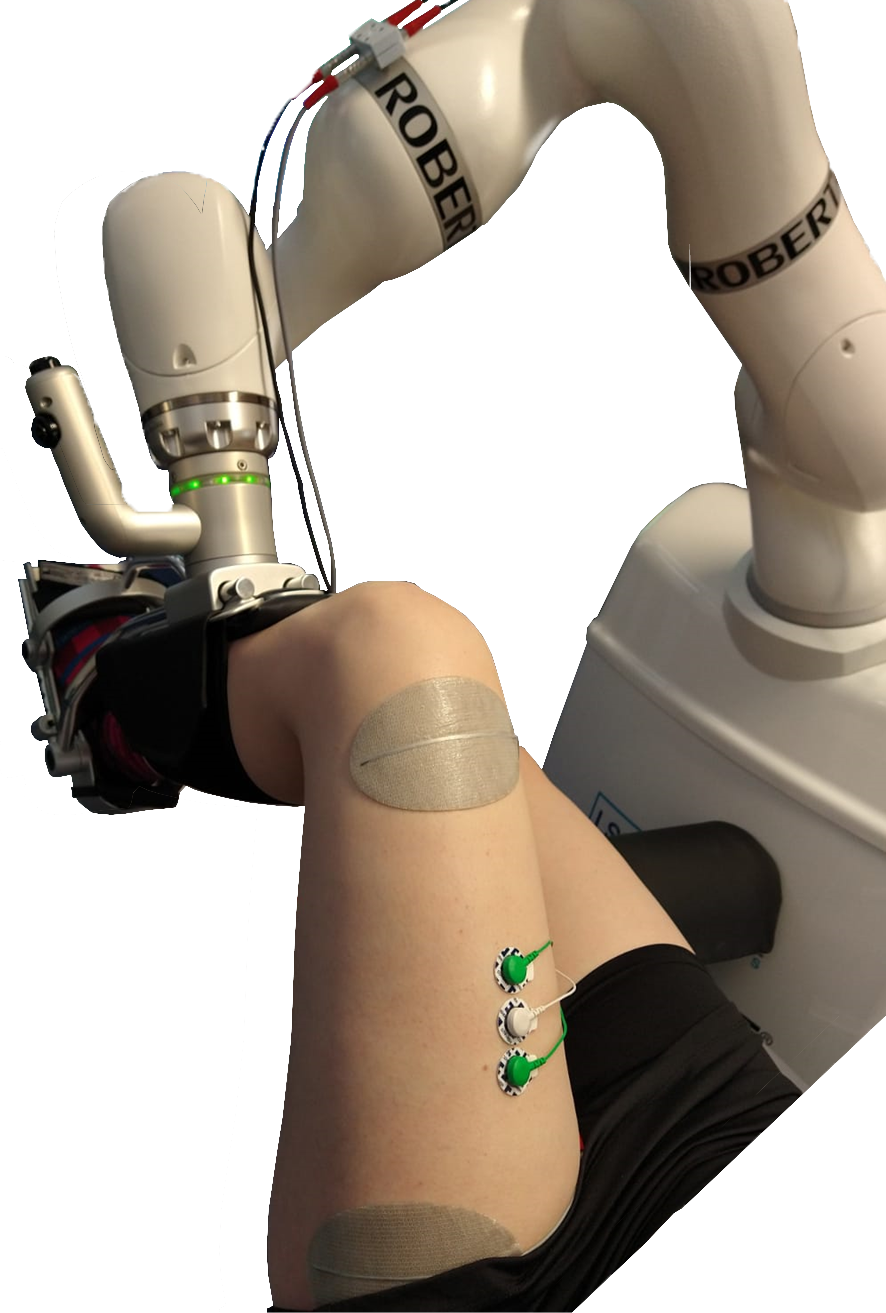
Over the past five years, Roessingh Research and Development (RRD) participated in the H2020 MyLeg project (http://www.myleg.eu), coordinated by Raffaella Carloni from the University of Groningen. Within this project, RRD was responsible for the high-level control of a to be developed powered transfemoral prosthesis. The ultimate goal of the project was to create a smart and intuitive prosthesis that was compatible with osseointegration. In adherence to the FAIR principles, all data that was gathered on individuals without an amputation have now been published as open access. We also published an open access article that describes the data which can be found here: https://www.nature.com/articles/s41597-023-02341-6. In this article we explain what we did, what the database is and where it can be found.
Intent recognition using EMG
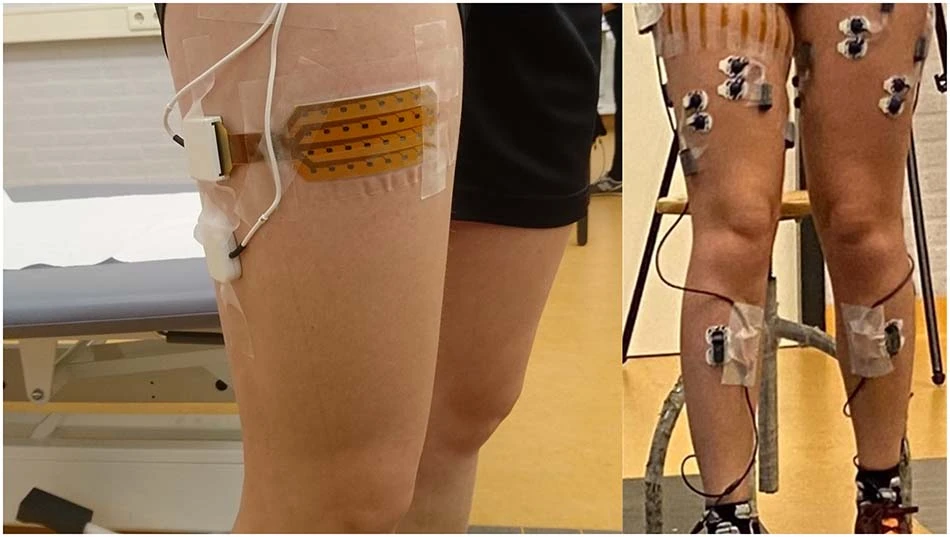
Surface electromyography (sEMG) is a non-invasive technique that could provide meaningful information for human motor intent recognition. Motor intent is the determination to move or change the state one is in. For instance, when we are approaching a staircase, we adapt our steps in such a way that we position our feet perfectly to ascent the steps. This intent can be captured using the signals that command our muscles to contract, precisely what sEMG records and analyzes.
The need for a lot of data
There are downsides to sEMG as well. sEMG suffers from confounding factors such as muscle fatigue, electrode placement differences and intra-subject variability. This means that a control schema that utilizes sEMG could work on one day, but could yield poor results on the next day. Therefore, a lot of data is necessary to capture the variability of sEMG between subjects and between days to develop robust human motor intent recognition systems. Furthermore, detecting the change from one activity to another is harder than detecting a continuation of the activity. Therefore it is necessary to have databases that are rich in these transitions so that algorithms can be trained properly.
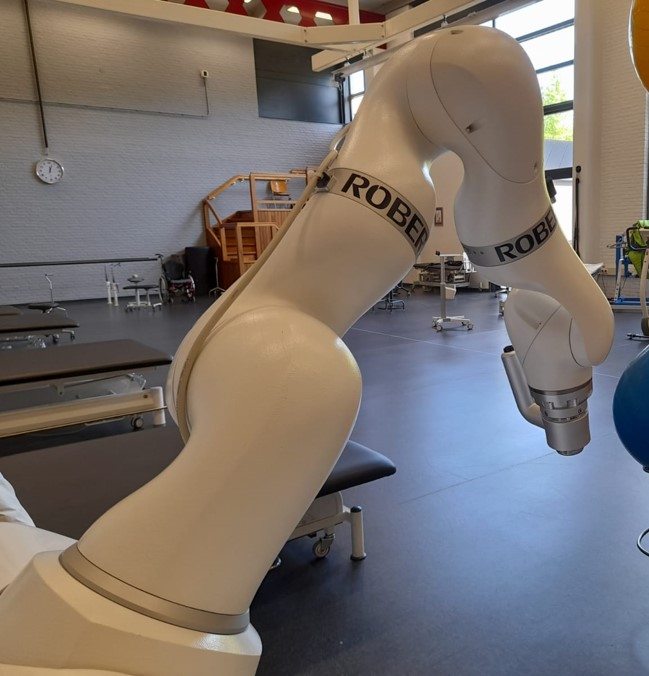
The RRD MyPredict database
In the past three years we have collected the Roessingh Research & Development-MyLeg Database for activity prediction (MyPredict), containing data from 55 subjects in 85 measurement sessions. These subjects performed all kinds of gait-related activities, including regular walking, traversing uneven terrains like grass, and climbing stairs, while transitioning freely from one activity to the next. During these measurements we collected kinematics and sEMG in various forms, using traditional bipolar sEMG as well as 64 channel multi-array sEMG.

The data it contains
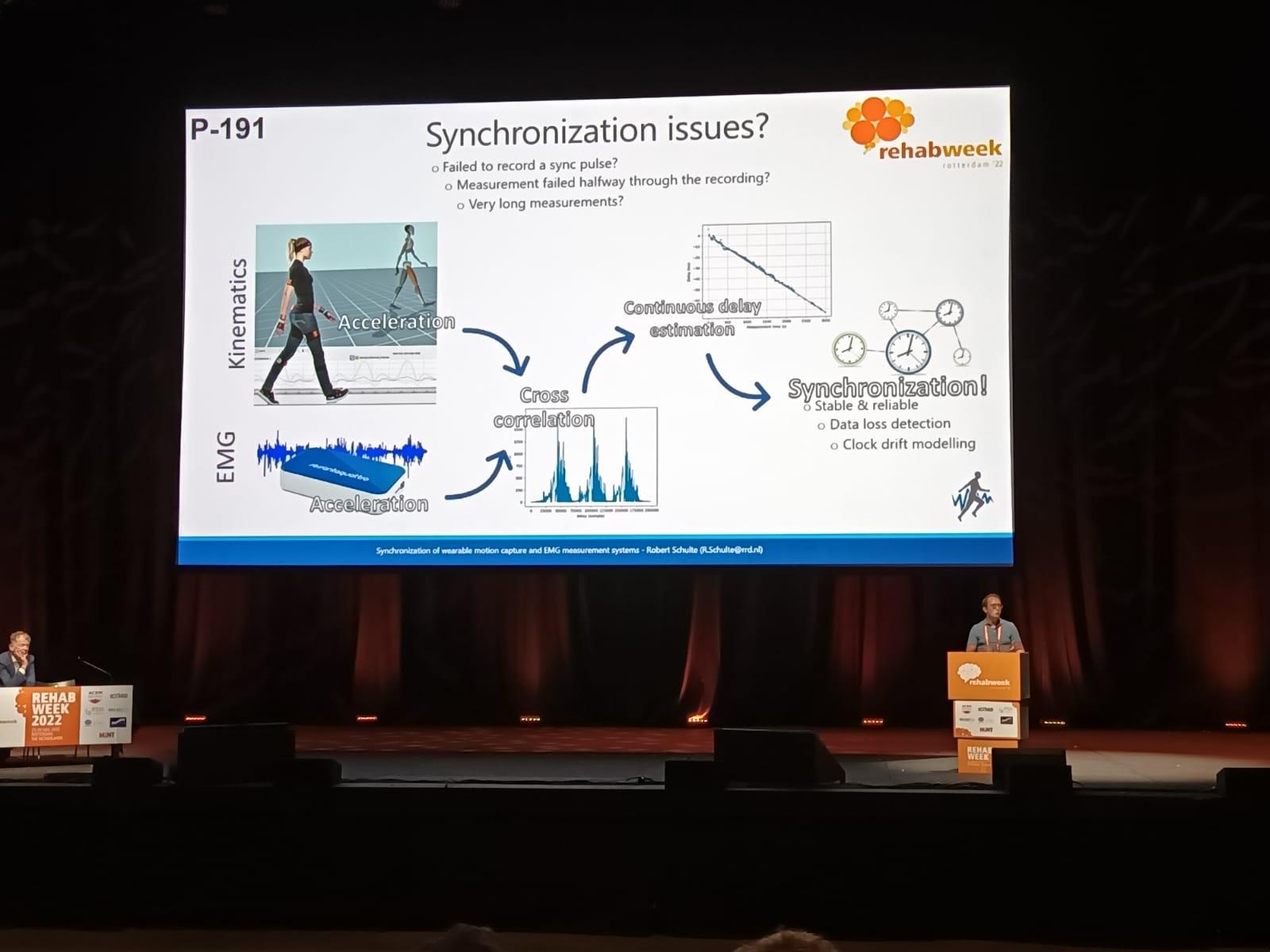
We have made use of wearable measurement systems, enabling us to measure easily inside the laboratory, but also outside. In this way we have a rich dataset containing gait activities in various settings. Next to that, we have measured 10 subjects on four different days in the span of one week. These measurements enables researchers to explore the impact of time and electrode placement on intent recognition systems, a critical aspect in improving the robustness and adaptability of these systems.
Data validation
An essential validation step involved comparing the MyPredict database with other publicly available datasets. The results of this comparison demonstrated excellent correlation, confirming the reliability and quality of the MyPredict database. In this way we have shown that this database can be a valuable resource to the research community.
What it can be used for
The MyPredict database provides an opportunity for researchers to delve into sEMG data and develop and refine intent recognition systems. This comprehensive dataset offers a foundation for further studies in the field of human motor intent recognition. Researchers can explore innovative algorithms, machine learning techniques, and signal processing methodologies to unlock the full potential of sEMG data. Ultimately, it is the goal to develop practical applications that utilize sEMG signals to enrich human-machine interactions.
Where to find it
The database is accessible via this link: https://doi.org/10.4121/20418720. Data collection was supported by the European Union's Horizon 2020 Research and Innovation Programme grant number 780871.