By Valentina Bartali and Monique Tabak
Four years ago, RRD (with different partners from all around Europe) started working on the European project BIONIC. In May, this project came to an end and, now, we would like to look back at our work and what we have achieved in these years.
The description of the project is written in this way: Personalized Body Sensor Networks with Built-In Intelligence for Real-Time Risk Assessment and Coaching of Ageing workers.
I can imagine that, from an outsider, with this description, it can be complicated to understand what BIONIC actually is.
BIONIC was a project aiming to develop a technological innovation able to detect real-time risks in the workplace (think, for example, about the industrial sector or factories) and in everyday life. Additionally, this technology has monitoring and coaching functions in order to help preventing musculoskeletal disorders. The system consists of a suit with sensors in different parts of the body, a smartwatch to measure heart rate and steps, and two applications. One application was developed to give feedback on the user’s movements, whilst the other application, Gamification app, was developed by RRD to motivate and coach users to live a healthy lifestyle, also outside the work environment.
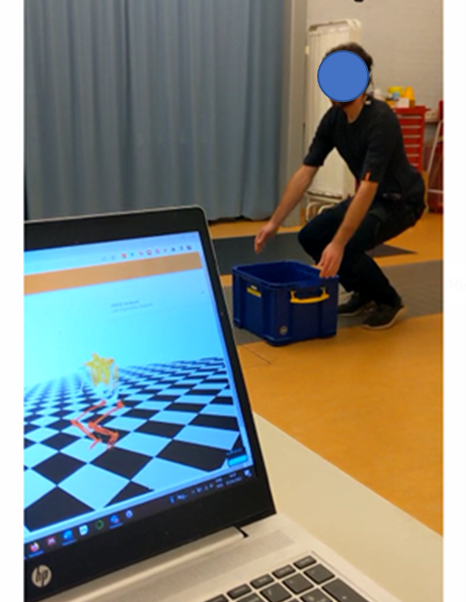

On the picture on your left, you can see how the suit is and what is shown on the computer. On the picture on your right, you can see the smartwatch and the application we created.
In BIONIC, our work was focused on estimating fatigue from sensors by machine learning algorithms (which you can read more about in the papers [1] and [2] in the reference list below) and the development of coaching strategies for healthy lifestyle for the gamification application.
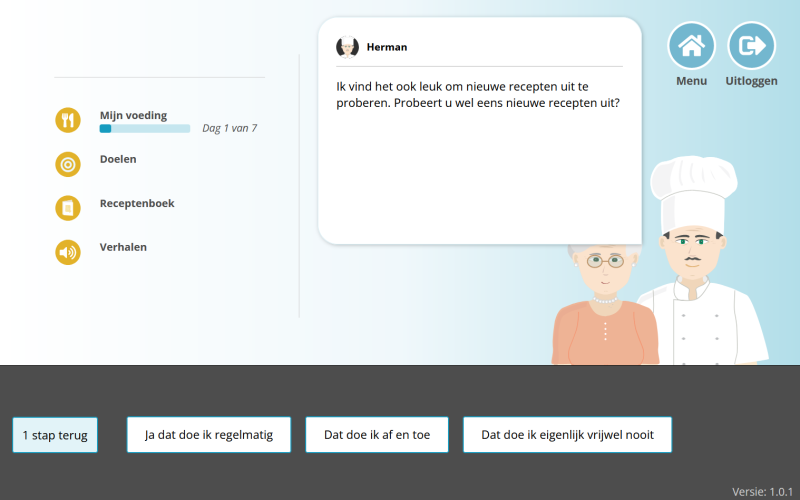
In this blog article, I would like to tell you a bit more about this gamification application we developed, which has the following components (to get a better idea, see video below):
- Overview of measured daily activity: users can get insights on their daily activities (step counts). The application (through an algorithm) can estimate the moments in which the user shows sedentary behavior (staying too much sitting) and the periods in which (s)he is doing some activity.
- Overview of subjective fatigue: every day, users will be asked, with a question in the app, how tired they feel that day. The answers to this question will be shown in a graph.
- Personalized exercise program: physiotherapy exercises advised to users in form of trainings and depending on which part of the body a user has the most issues (for instance, back, neck, or legs).
- Motivational support via virtual coach Bill and gamification elements: Proposing physiotherapy exercises according to the feedback received from the BIONIC system and the needs of the users. These exercises are given by a virtual coach, Bill, who guides, motivates, and supports users. The Gamification App has gamification features to prompt users to do the exercises proposed and to change their physical activity (when needed). These gamification features entail earning points through:
- Challenges: a set of goals that the user can set up for him-/herself
- Achievements: a set of tasks that the user can achieve whilst using the Gamification App
The Gamification App was also evaluated in clinical settings at Roessingh to investigate if this technology could be of added value. From this evaluation, we discovered that the application could really help patients to be more aware of their activity patterns and it could motivate them to change their activity behaviors and facilitate rehabilitation.
We are really proud of what we achieved in these years considering that we were able to develop a working application of which added value was seen. The project is now finished, but we will bring with us what we have learnt during these years and we hope to further develop and use the application for other purposes.
Reference list
[1] Marotta L, Buurke JH, van Beijnum B-JF, Reenalda J. Towards Machine Learning-Based Detection of Running-Induced Fatigue in Real-World Scenarios: Evaluation of IMU Sensor Configurations to Reduce Intrusiveness. Sensors. 2021; 21(10):3451.
[2] Marotta L, Scheltinga BL, van Middelaar R, Bramer WM, van Beijnum B-JF, Reenalda J, Buurke JH. Accelerometer-Based Identification of Fatigue in the Lower Limbs during Cyclical Physical Exercise: A Systematic Review. Sensors. 2022; 22(8):3008